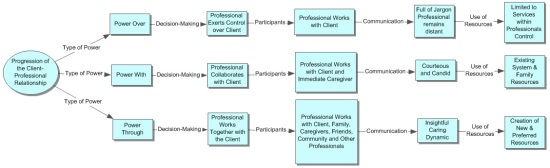
When writing the initial blog post “How to we get to Client-Centered Practice,” I fully intended to include something on the evolution of the client-therapist partnership. Unfortunately, I did not so I felt that it was important to write a second post. I had read this book, oh so long ago, when I was working in early intervention home care. I felt that the evolution of the therapeutic relationship was as important then as it is now. I feel that in many ways, doctors and therapists are still vacillating between levels of power, decision making and communication. I personally feel that all doctors and therapists need to get to the level of shared decision making with insightful, caring and dynamic decision making. Two words come to mind: Authoritarian and Authoritative.
When a therapist acts in an authoritarian manner, the therapist is in total control of the session with no input from the client. The phrase, “My way or the highway” comes to mind. When a therapist acts in an authoritative manner, the therapist imparts his or her knowledge with input and feedback from the client. It does allow for the sharing of knowledge and resources for both the therapist and the client. So from the 1950’s to the 1960’s, professionals tended to exert control over clients. This was when doctors and therapists were ‘gods’ which still remains today in older patients. Moving into the 1960’s through the 1970’s, the client patient relationship became somewhat more collaborative. Professionals became more candid and courteous with some changes to the level of jargon in documentation and conversation, although in my opinion, professionals remained authoritarian. As we come into the 1980’s, authoritarian was still the rule but there was more family involvement. The family became a resource to help the client and began being involved in the treatment process. From the 1990’s to today, authoritarian has become authoritative, with professionals finding new and innovative ways to manage patient care. P4s were developed to help the physician become more in tune with the needs of the client and involve the client in leading changes to effect better healthcare management.
So while there are changes happening, we are still stuck in the mindset that we grew up with and inherited from our parents. I believe that it is this mindset that effects how patients perceive physicians and therapists. It is our duty to help change the ways in which we deliver therapy services; change the way that we interact with clients; the ways in which they perceive us; in having responsibility for progress; and engage our clients in advocating for themselves.
