I recently read a well-written and well-thought out post by Brock Cook, an esteemed colleague from Australia, “Who are we trying to convince? A reflection on client-centered practice.” He was writing on the conundrum that we face as therapists trying to achieve the ultimate of client-centered practice. I believe that client-centered practice can be achieved but not in the literal sense, particularly when reimbursed through a 3rd party payment system. Due to the reimbursement structure, clients do not necessarily get to pick their goals. Goals are based on the treatment setting and reimbursement structure. I believe that the label “client-centered practice” is not actually correct. I feel that the term, “client-therapist partnership” is more in line with engaging the client in the therapeutic procedure. We need to think in terms of systems, much like P4s. In the medical model, P4s are based in systems biology. In the medical model, the terms in P4s can be defined in the following manner:
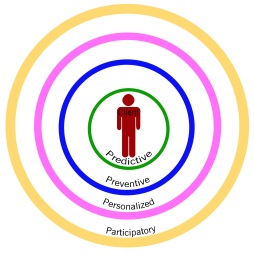
- Predictive: Predicting the emergence of disease “networks” within the individual patient. Organ-specific proteins found in the blood will be analyzed in a longitudinal manner across the individual’s life. Changes in baseline measurements at the molecular level will enable early disease warning.
- Preventive: Preventive medication- We may be able to predict the potential future emergence of disease-perturbed networks in patients and then design “preventive drugs” that will block the emergence of these disease-perturbed networks and their cognate diseases.
- Personalized: Each person is genetically unique and must be considered as a unique individual—not as a statistical average.
- Participatory: Activated and networked consumers will do more than demand more effective healthcare–they will help lead the changes necessary to achieve it. [http://p4mi.org/4-ps-quantifying-wellness-and-demystifying-disease]
So how do the P4s impact on occupational therapy services? Technically, we can use the same terms to define the scope of our practice. What can we predict about the client’s level of function based on his or her diagnosis? And their level of function prior to the current illness or disability. Does that mean that the therapist focuses on the disease and not the patient? What can we do to prevent further disability? How do we personalize our therapy session so that each is unique to the individual client? How can our clients participate in the decision making process with regard to their current and future treatment?
Based on Mr. Cook’s research for his post, he identified the following concerns based on barriers to goals and goal setting; consumer perceptions; barriers within the medical model vs. a wellness model; therapeutic relationships between clients and therapists:
- the therapist and client have different goals
- the therapists’ values and beliefs prevent them from accepting the clients’ goals
- the therapist is uncomfortable letting clients choose their own goals
- occupational therapy environment as contrived and as limiting choices and opportunities for exploring personally meaningful occupation
- focus upon the illness rather than the individual served to diminish any partnership between the client and therapist
- exclude the client from decision-making processes
- promotion of client-centered occupational therapy may be more possible outside of the medical model and within the framework of health promotion and wellness models
- the client in the client/service provider relationship
- the client in the social and mental health system
- client-centered care means I am a valued human being
- negative attitudes and stigma
- an indifference to them as human beings
- a status differential between themselves and service provider
- a lack of trust
- the use of intervention techniques that did not meet client needs
- fear of hospitalization
- fear of anger from service providers if they complained
- fear of their illness
- disillusionment with service providers
- poor self-esteem
- feelings of marginalization
According to Mr. Cook, much of this literature, that he has reviewed for his blog post, attempts to clarify the definition of client-centered practice and considers the patients as subjects in studies and not as clients.
Having had professional experiences that include many of the concerns identified by Mr. Cook, I decided to begin my own research in client-centered practice. Needless to say, as Mr. Cook expressed so eloquently, many therapists feel that they have a handle on exactly what client-centered practice is and feel that they are either thoroughly engaged in the process or not. Mr. Cook’s post seems to suggest, there is a discrepancy between what is allowed as a goal, either by the therapist’s restrictions or that of the facility and the 3rd party payer. Based on these restrictions, therapists must work on goals that will demand payment for services. Let’s face it, we all need to make a living. Does that mean that our clients never get to work on goals of their choosing? No, not really.
We must assess our client’s skills based upon the treatment setting. If we are working with students, the goals must be educationally relevant. Potentially, we may not even have occupational therapy goals but collective goals developed during the CSE meeting. In a hospital setting, much of our work is centered on self-care, transfers, safety, energy conservation, etc. So you know the drill. Goals are created for the client based on the treatment setting and his or her disability. It really sounds like a disease oriented system and not a client oriented system. That may not be quite true either. But how can that be? According to Linda Tickle-Degnen, PhD, OTR/L (2002), client-centered practice includes respect for and a partnership with the people who receive our services. This respect and partnership supports the development of the therapeutic relationship which is the basis for client-centered practice.
The therapeutic relationship, based on Ms. Tickle-Degnen’s work, within the client-center practice concept includes the following:
Developing a rapport between client and therapist in which the individuals grow to like one another and experience each other as generally warm, respectful and understanding. Personally, I am not trying to win any popularity contest. I don’t need my clients to ‘like’ me or ‘love’ me. I do need to present myself as someone who will empathize with them and provide them good services.
- Developing a working alliance which includes collaboration with one another to develop common goals and a sense of shared responsibility while working on tasks to achieve those goals.
- Maintaining that working alliance through difficult changes and challenges that occur in therapy.
- And my own addition to the therapeutic relationship is that clients need to be able to self-monitor and see progress outside of therapy. To that end, I use rubrics. I instruct the client in the structure and use of each rubric. A client needs to know what my expectations are and that I will modify their therapeutic program to ensure the achievement of the goal.
Much of my work has been in secondary school-based therapy. In my opinion, you must be able to engage your students in the therapeutic process. If you are unable to do that, you will lose them. In this instance, with older students-many of whom have been in therapy since pre-school, it is imperative to gain their ‘alliance.’ One way that I have gained their alliance is by giving the student the opportunity to have a say. By this age, many students are feeling the need to be more autonomous. They would like to have less teacher supervision and oh yes, less or no therapy.
I need to report on function but I also must include the input from the student. I believe that the student needs to be part of every aspect of the development of the IEP. I believe that a student needs to participate in each meeting that occurs on his or her behalf. When students are not given the opportunity to participate, their responses tend to include some of those exact same concerns that Mr. Cook expressed in his blog post:
- a status differential between themselves and service provider
- a lack of trust
- the use of intervention techniques that did not meet client needs
- fear of anger from service providers if they complained
- disillusionment with service providers
- poor self-esteem
- feelings of marginalization
In therapy sessions, while working on either vocational or educational goals, one of the tasks that I include is to develop a portfolio of skills and goal progress. Sometimes, this portfolio is electronic and other times it is a paper portfolio. The type of portfolio depends on goals. If keyboarding is included in the goals then it is always an e-portfolio. Having the opportunity to demonstrate preferred activities provides a sense of accomplishment and awareness. A sense of accomplishment of what they have achieved and a sense of awareness of where they need to go. I also have the students create a resume and predict where they would like to be in 5 years, 10 years, etc. Sometimes, the students would like to include a video and I encourage them to do that. By working in this manner, many students come for “extra” therapy during lunch times.
So how do I get my students engaged? I will tell you. It is important, from day one, to gain your student’s trust. If this is a new evaluation, I perform the evaluation over the course of a week or more. CSE meetings do not generally occur immediately after the referral, so I have some time. I ask the student to complete The Student Interview. This provides me an enormous amount of information on the student’s function both in school and at home. This interview provides the student the opportunity to describe what is working for him or her and what is not. This is a tool for developing those ‘common goals’ within the educational model.
I also use a number of ‘authentic assessments.’ I use a number of assessment rubrics for real world tasks that the student must perform during the school day. Once I have completed an assessment rubric, I share the results with the student. This provides the student with the criteria that I used to assess the skill. It also gives the student the opportunity to give me feedback on his or her performance and their understanding to the task. For an explanation of rubrics and occupational therapy, please refer to my book Using Rubrics to Monitor Outcomes in Occupational Therapy.
So I feel that including the student in the evaluation process and in ongoing goal progress monitoring, my students know that they are valued members of the CSE Team and can voice their opinion, wants and needs. I prep my students to participate through interview, progress monitoring and a portfolio of skills. Even when my students are hesitant to speak or unable to speak, they [and I] have a number of resources to fall back on. I believe that I am already engaging in client-centered therapy, to the best of my ability. I want my clients to know I have their back, even though we may not be friends.



You must be logged in to post a comment.